Frozen shoulder (adhesive capsulitis) occurs when the capsule (consisting of connective tissue that surrounds the shoulder) thickens and contracts. This leads to stiffness and shoulder pain with restricted movement.
The capsule is a balloon like structure that surrounds the shoulder (glenohumeral joint). It is usually very loose to allow the shoulder to move in all directions. Lining the inside of the capsule you will find synovial cells which produce synovial fluid which in turn provides nutrients to the joint lining cartilage. The capsule has a series of thickenings which also help keep the shoulder in joint (The superior, middle and inferior glenohumeral ligaments) and stop the shoulder dislocating. The glenohumeral joint capsule actually maintains an internal vacuum which keeps the ball and socket of the joint near each other.
The negative pressure stops the shoulder dislocating even if the muscles are not actively contracting to keep it in joint. This is one of the reasons our shoulders do not dislocate when we sleep or after we die.
Adhesive Capsulitis
Adhesive Capsulitis is common and affects 3% of the population. While we don’t understand why the condition happens we do know the typical pattern that it follows. It most commonly affects people over the age of 40 years, in women far more often than in men. It may be triggered by an injury or previous surgery (heart or breast) but it is also associated with a range of medical conditions including diabetes, thyroid disease, high cholesterol and inflammatory disorders. There is probably an auto-immune component involved. It occurs in both shoulders in 10-20% of individuals. This condition is characterised by specific phases which overlap. Overall though, frozen shoulder is a self-limiting condition which may take up to two years to resolve.
There are 3 distinct phases to a frozen shoulder:
- The FREEZING PHASE lasts about 2 to 9 months (sometimes even longer in diabetics). Patients get pain at rest, with activity and also pain at night. There is significant restriction of motion and pain occurs with movement of the shoulder. Sleep can be very difficult.
- The FROZEN PHASE displays progressive stiffness, lasting up to 12 months. Pain occurs only at the extremes of movement but the shoulder remains stiff. Range of motion typically diminishes greatly. Sleep usually improves at this stage.
- The THAWING-OUT PHASE is the resolution phase where movements improve over a 12 to 24 month period. This phase is not typically painful and the shoulder’s range of motion slowly returns towards normal.
The goals of most frozen shoulder treatments are to retain as much range of motion in the shoulder as possible as well as to control pain. In 80% of patients the pain resolves completely but some people are left with a small and permanent restriction of range of motion. This loss of motion does not usually cause any long term problems.
In the early stages a frozen shoulder can be difficult to differentiate from other causes of shoulder pain and stiffness. By six months the diagnosis is usually very clear clinically. Other conditions which can cause pain and stiffness in the shoulder include osteoarthritis, impingement and calcium deposits (calcific tendonitis).
In most cases the only investigation required is a plain x-ray. This will rule out most of the above conditions.
A stiff shoulder after an injury or surgery is often referred to as a frozen shoulder but is not in fact adhesive capsulitis. Adhesive capsulitis is a self limiting condition which gets better with time and does not require much in the way of physiotherapy, stretches or releases. A postoperative stiff shoulder will stay stiff forever unless appropriate exercises are initiated early and diligently under the supervision of a physiotherapist.
Treatment
The most important aspect of the treatment is to understand that this is a condition that should get better by itself. The mainstay of treatment is to use the shoulder as much as possible (but within the limits of your discomfort). It is important not to immobilise the arm or stop using it, as this will cause the condition to deteriorate.
Medications
Medications do have a role and these include analgesics (pain killers), anti-inflammatories and sometimes medications to assist with sleeping. There is a large range of medications which vary in their effect between individuals. One of the drugs that seems to work for most people and seems to have few side effects is Mersyndol (a combination of Paracetamol, Codeine, Phosphate, Hemihydrate, Doxylamine Succinate). Many people are given cortisone injections into the subacromial space (bursa) before the diagnosis becomes clear. These do provide partial relief for some people for a short period of time but generally do not make much difference.If you are struggling to sleep, a cortisone (steroid) injection into the glenohumeral joint often reduces the pain at night for 6-8 weeks and can get you through the worst of the process. These injections are usually given under ultrasound or CT guidance and using a sterile techniques because there is a small chance of getting an infection any time a joint is injected.
Physiotherapy
Has a very limited role (depending on the phase of the frozen shoulder). Exercises are used to maintain movement and strength but must not cause pain. The exercises are not designed to restore your range of movement. The aim of the exercises is to keep the shoulder mobile and avoid further stiffness. Aggressive and painful manipulation of the shoulder usually aggravates the condition and should be avoided. Once the pain has gone it is worth visiting a physiotherapist to learn a home exercise programme to strengthen the upper back (periscapular) muscles as well as the rotator cuff.
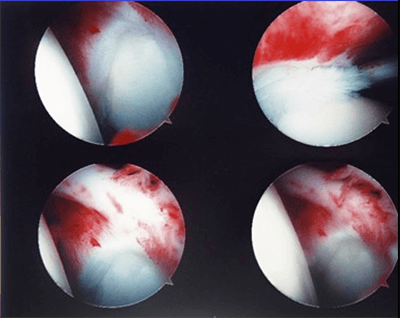
Hydrodilation (also called hydrodistension) and Post-Injection Stretching is an injection and stretching technique where a Radiologist “blows up” or distends the shoulder joint with fluid, and breaks down the contractures. The aim is to advance the patient more quickly through the stages of frozen shoulder and works well for some patients. The aim of the procedure is to break the cycle of inflammation and release the contraction of the thickened joint capsule. I suggest taking some pain killers before you go for the procedure to make it more tolerable. This should only be done by an experienced radiologist and ideally you will feel a pop as more and more fluid is injected into the shoulder. Before this there will be a build up of pressure and pain which goes away when the capsule ‘bursts’. Immediate stretching is commenced and continued for about 4 weeks. The regime of post-injection stretching is important and involves using the ‘good’ arm to assist in stretching the injured shoulder. Use the shoulder and arm as usual within pain limits. The shoulder should not be nursed.
The risks and side-effects include post-injection pain (up to 3 days), infection (1:15,000) and allergy (1:100,000). If you have not reached the “frozen” phase within 9 to 12 months, then there is a reasonable case to perform a Manipulation under Anaesthetic and an injection of cortisone. This requires an admission to hospital for a few hours and a general anaesthetic. The shoulder is manipulated and injected with cortisone under sterile conditions. Following the procedure you will require 3 to 4 months of physiotherapy. The success rate of the procedure is 70% but there is a 2% chance of breaking your arm during the manipulation. The other risks are those of the anaesthetic and infection into the joint with the injection.
Surgical release of the capsule can be done but is not without risk. The procedure is done arthroscopically under general anaesthetic with a complete release of the joint capsule followed by physiotherapy in hospital. The axillary nerve can be permanently and irreversibly damaged which can affect the ability to lift the shoulder in the air. While this is rare it is potentially a devastating injury for what is usually a reversible condition. The results of this procedure are generally better than those of a manipulation alone. In most cases I suggest you learn to live with the condition for 12 to 24 months – (providing the pain is tolerable and you can cope with the activities of daily living).
FAQs
Adhesive Capsulitis is common and affects 3% of the population. While we don’t understand why the condition happens we do know the typical pattern that it follows. It most commonly affects people over the age of 40 years, in women far more often than in men. It may be triggered by an injury or previous surgery (heart or breast) but it is also associated with a range of medical conditions including diabetes, thyroid disease, high cholesterol and inflammatory disorders. There is probably an auto-immune component involved. It occurs in both shoulders in 10-20% of individuals.
Understanding the condition is the most important thing to do. It is a self limiting condition which will get better if you wait. Treatment is designed to relieve pain and help you sleep. This varies from anti-inflammatory tablets or pain killers to injections and as a last resort surgery.
Both injections go into the glenohumeral joint and both contain local anaesthetic and cortisone. The injection is typically a 3-5ml injection which is designed to act as a topical anti-inflammatory medication. The hydrodilation is designed to stretch and possibly tear the joint capsule and involves injection as mcuh fluid into the joint as the patient can tolerate from a pain perspective or until a pop or release of joint pressure is felt.
Both procedures to have an element of risk in terms of infection, allergy or damage to the joint capsule.
Physiotherapy generally makes things worse in the early stages of adhesive capsulitis as it stretches the irritated capsule. It can be useful once the pain has settled but most people simply start to use the arm and restore the motion naturally. A home stretching programme can be useful after a hydrodilation procedure.