Shoulder arthritis causes pain and loss of movement in the shoulder. The joint lining cartilage wears out and the bones rub against each other. These days we have the technology to be able to do a shoulder replacement (like we can do hip or knee replacements) to relieve pain and restore function to the shoulder. The type of prosthesis that is inserted will be determined by the amount of bone available to accept the components and whether the rotator cuff muscles are intact or not.
In the situation where the rotator cuff is torn we know that a regular shoulder replacement will fail. In this situation we need to change to a prosthesis that does not rely on the rotator cuff for stability or movement.

In a reverse total shoulder replacement procedure, the ball and socket sides of the joint switch places.
In a normal shoulder the deltoid (top shoulder muscle) pulls the humerus superiorly (upwards) while the rotator cuff balances the pull inferiorly (downwards). The rotator cuff also initiates forward elevation (lifting the arm in front of the body) and abduction (sideways) movement of the shoulder before the deltoid takes over and completes the movement. When the rotator cuff is torn the humeral head is pulled upwards only and ‘escapes’ anteriorly and superiorly (out the front).
The first reverse shoulder replacements were performed in the 1970’s and had many problems. Many lessons were learned from this and design modifications were undertaken to change the centre of rotation of the shoulder joint to allow the deltoid to provide movement and stability for the prosthesis and bypass the rotator cuff.
The complication rate of this operation is now low when performed by experienced surgeons. For difficult cases, Surgeons are now able to use computerised patient specific instrumentation, where a computer designs specific instruments based on a CT scan of the patient , that allows the surgeon to place the components of the replacement in exactly the correct position.
Reverse shoulder replacement is now an excellent alternative for patients with rotator cuff arthropathy (arthritis from their rotator cuff tear) or other conditions where there is failure of a total shoulder replacement or where the shape of the socket of the shoulder is abnormal due to previous surgery or a congenital deformity.
Use of the arm is started the day after the operation and a sling is worn at night time only for 4 weeks after the procedure. Physiotherapy is usually not needed with reverse shoulder surgery.
It is important to note that this procedure does not restore the ability of the shoulder to perform heavy work or sport.
PATIENT INFORMATION Handout
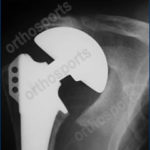
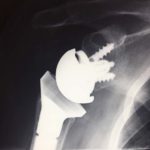
Xrays of cases usually treated with a reverse shoulder replacement
FAQs
Arthritis is far less common in the shoulder than it is in weight bearing joints like the hip and knee. If your rotator cuff is torn then the ball of the shoulder can ride up out of the joint and start to rub on the acromion bone and also the glenoid bone. This wears away the joint lining cartilage and causes pain and stiffness in the shoulder (arthritis).
The rotator cuff muscles start the shoulder moving and then the deltoid muscle takes over the rest of the movement. If the rotator cuff is torn then it is impossible to start the movement in the first place. After surgery this should be significantly better but not all patients can get their arm all the way up again.
Most patients are in hospital for 2 -3 days after surgery. There is no physiotherapy required so as soon as your pain is controlled you can go home.
Most patients simply start to use their arm after the operation. Typically you will wear the sling at night time (and occasionally during the day) for the first 4 weeks. You may use the arm for simple daily activities like feeding and washing the day after the operation in most cases. Physiotherapy is only required if you have not achieved adequate function at about 3 months after the operation.
The joint replacement is made of a various metals combined together which are relatively inert and well tolerated by the body. Metal is placed in the humerus as well as being attached to the glenoid bone. Between them is a high grade medical plastic called polyethylene which allows friction free movement between the components. This can wear out after many years so you will need to have regular xrays performed to ensure that the prosthesis continues to function well. Changing the plastic liner is a relatively easy procedure with little down time but with the modern technology is rarely necessary.